The first thing that we need to say is that this is the approach that was taught to us by the legendary Dr. Ravi Morchi at Harbor UCLA Medical Center. All the credit for this lecture goes to him. This is the approach we still use when faced with the undifferentiated hypotensive patient.
Now let’s get going.
Imagine you’re in the ED or better yet you are the cross cover intern on gmed nights when you get a page from a nurse at 3 AM. You call the nurse back and he tells you that a patient who you don’t really know is suddenly hypotensive with a sbp of 65. After you wipe the mounting bead of sweat off of your forehead, what do you do?
The first thing you’ll need to do is fight the instinct to go chart reviewing for the next 30 minutes. Instead the first thing you should do is run over to the patient’s bed and... be sure to take your ultrasound with you.
When you arrive at the room don’t spend a lot of time talking to the patient. Ask the patient what his/her name is in order to ensure that the airway is protected. Now that you’re done with that formality, follow the following steps to begin resuscitation as soon as possible. Once you have initiated resuscitative efforts then take the time to talk to the patient and do a quick chart biopsy.
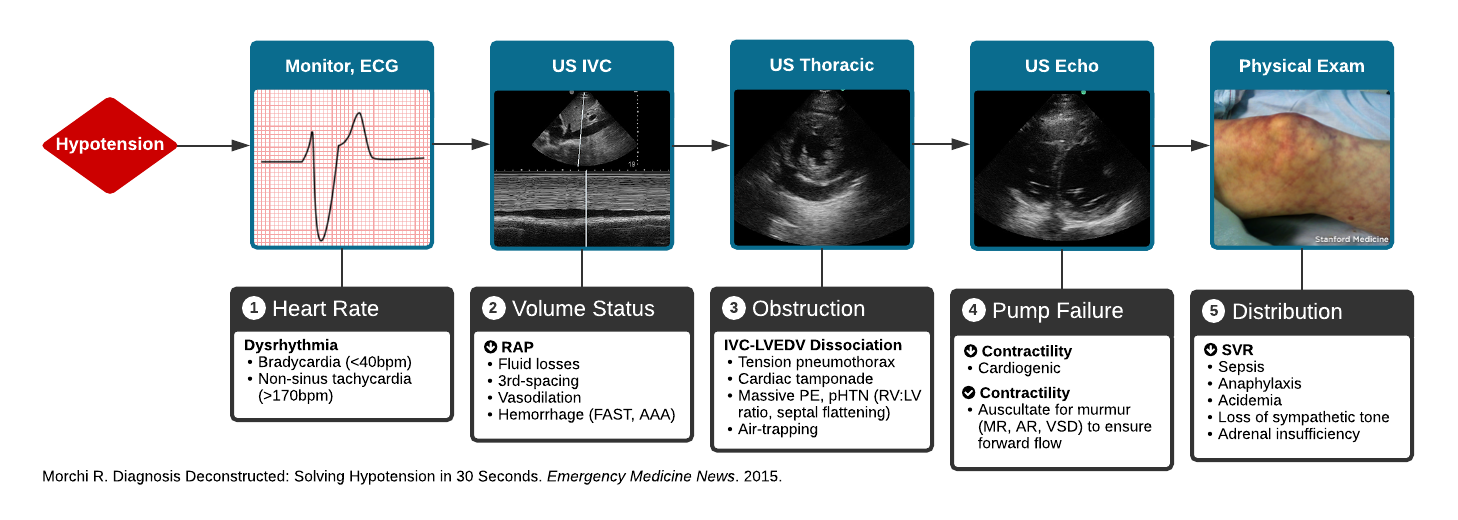
STEP 1: Look at the Monitor
Is the patient’s heart rate too fast or too slow. Ask yourself, do I need to cardiovert this patient or pace them?
What’s too fast? Usually you will start thinking about cardioverting the patient once they have a hr > 150.
What’s too slow? Usually you will start thinking about going down your bradycardia algorithm once the patient has a hr in the 30s.
STEP 2: Look at the Heart with the US
The questions you want to ask yourself are:
Is there a pericardial effusion. If so and the patient is hypotensive get ready to perform a pericardiocentesis
Is the EF OK or is is crap. Consider trying to get a parasternal long view to see if the mitral valve hits the intraventricular septum. If it does the EF should be OK. If you see that the EF is shit then you know that you are probably dealing with a CHF exacerbation
Is there Right Heart Strain. Like all things you are going to want to consider PE. If you see Right Heart Strain you may need to consider pushing TPA.
STEP 3: Look at the IVC
(Before we continue we want to point out the IVC has been shown to not be the most reliable marker of volume status. There are a lot of false positives and negatives that occur. but with that said when your back is against the wall it’s a decent starting place until better things come along).
Ask yourself is the IVC Plump and not moving with respiration or is it collapsible.
At this point take a second and put together the information you have with Step 2 and Step 3.
OK EF with hyperdynamic heart + collapsable IVC = give fluids. The patient is probably intravascularly dry and needs ivf.
Poor EF + Dilated IVC = Diurese the patient. The patient is probably in cardiogenic shock (on the opposite side of Starlings curve) and needs to get that excess fluid off
STEP 4: Do an EFAST Exam
Any free fluid fluid in the belly should be tapped if possible. If the patient is anticoagulated or a cirrhotic you may pull out blood that would represent hemoperitoneum. Call for blood and possibly a surgeon. Maybe you find that the patient has SBP and there is a life threatening infection that needs to be treated.
Look at the lungs and make sure you are aren’t missing a tension pneumothorax
STEP 5: US the Aorta
Don’t miss a AAA or an Aortic dissection
At this point you have either stuck a needle in the heart, pushed tpa, given IVF, taken fluids off, started a massive transfusion protocol, or found an Aorta that has exploded. You have officially begun the resuscitation and done all the things you possibly can to stabilize the patient. And hopefully as you get better at your ultrasound skills you’ll be able to make these decisions within 5 minutes of getting to the bedside. Now that the resuscitation has started talk to the patient more, do a chart review, and figure out if you need to start pressors or other life supporting measures. This is a good algorithm to follow even in the transiently hypotensive patient (lecture on this topic to come soon).
ddxof.com Algorithm for Hypotension
Full ddxof.com article on hypotension can be found at https://ddxof.com/hypotension/
Subscribe to the EM Ed by entering your email in the subscription box below. Don't rely on Facebook to get notifications for new posts. We only email when a new post is published. No spam. If you are reading this on your phone, just keep scrolling down to get to the Subscribe box.
Give us some love by sharing the EM Ed with people you think would like it. Post the lecture on social media. Like and Follow our Facebook Page. Follow us onTwitter. Follow us on Instagram